What’s Causing My Heel Pain?
Heel pain is a common, often disabling condition. Heel pain, well sucks. Heel pain affects approximately
10% of the population. That’s about 98,000 people in Edmonton alone! Heel pain is often associated
more with runners and older adults.
People often ask us, “Why does my heel hurt?” There are multiple causes of heel pain. Below we’ll discuss some of the more common causes of heel pain, what you can do about it, and how REP Physio can help. The information below is for informational purposes only. As always, if you have questions about your health, see a health professional, such as the physiotherapists at REP Physio.
Heel Pain Cause #1: Plantar Fasciitis (PF)
What is it?
The plantar fascia is a broad, supportive piece of tissue that extends from the heel (calcaneus bone) to your toes. The plantar fascia provides support for the arch of your foot and helps with your foot’s biomechanics. Plantar fasciitis occurs when this tissue begins to break down, typically when the “load” through the tissue exceeds its capacity. PF is the most common cause of heel pain.
What causes plantar fasciitis and what are the symptoms?
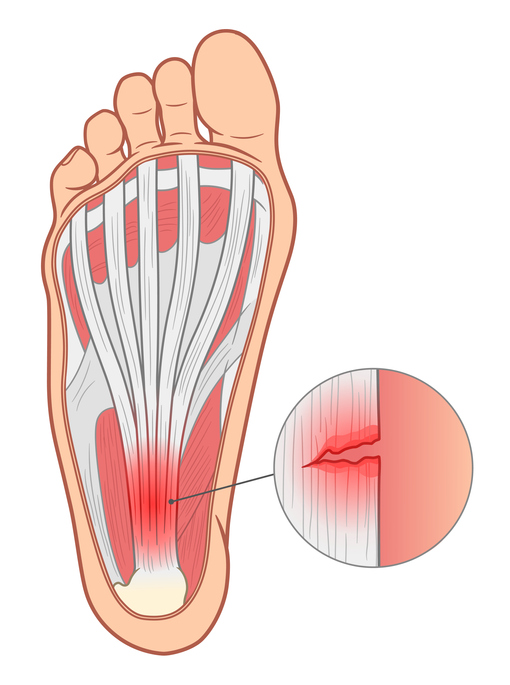
Plantar fasciitis (PF), which is sometimes referred to as plantar fasciosis, is usually an overuse injury. Clinically it is typically correlated with a rapid increase in activity over a short period of time. This “overuse” or “mechanical overload” could be as simple as taking a job that involves a lot of standing when you were used to sitting at work. It can also occur when starting a new running/exercise program too quickly and not letting your body adapt to the increased demand/load. Other factors that may predispose you to PF include the shape of your foot (high/flat arches), recent weight gain and a lack of range of motion at the ankle into dorsiflexion (moving your toes to nose).
PF pain tends to be localized to the heel/bottom of the foot, typically towards the front and inside (big toe) portion of your heel bone. The pain can also extend towards your toes. Plantar fasciitis heel pain is typically worse first thing in the morning but can get better after walking. The pain tends to lessen when you are off your feet, or are wearing supportive comfortable footwear. Plantar fasciitis also tends to affect only one foot at a time, not both.
One way to see if your heel pain is due to PF is to walk on your toes for a few steps first thing in the morning when your heel pain is at its worst. If the pain is still there with toe walking, then there’s a good chance that it might be plantar fasciitis. If the pain lessens/goes away, then it might be due to muscle shortening in the “calf” (see cause #3 below).
Do I need an X-ray for plantar fasciitis?
Generally, no.
In some cases, if your heel pain symptoms have persisted for 6+ months your physiotherapist at REP Physio can further discuss your suitability for imaging. Typically, an X-ray and/or diagnostic ultrasound is performed. A diagnostic ultrasound can determine if your plantar fascia has micro-tears that may require further treatment options, including referral to other health care providers which the therapists at REP Physio will happily do. Surgical intervention for plantar fasciitis is almost unheard of.
What if an X-ray shows a heel (plantar) bone spur?
Don’t worry. Heel spurs are common in the general population, and their incidence increases with age. One study has found over 40% of people aged 70+ had a heel spur. While heel spurs can be associated with heel pain, the presence of a heel spur does not mean that it is actually the spur that is causing your pain. Heel spurs found on X-ray are often deemed to be incidental findings. Said differently many people can have heel pain without having a heel spur, and many people can have a heel spur without any heel pain.
What can I do to fix my heel pain from plantar fasciitis?
At REP Physio in Edmonton, we use an active, evidence-based approach to heel pain. This typically involves education about potential activity modification, tips about comfortable footwear, a regular stretching and strengthening program as well as intramuscular dry needling (IMS) and/or radial shockwave therapy. For some examples of stretches/mobility exercises for plantar fasciitis and heel pain in general see the video link below.

Are you suffering from heel pain or plantar fasciitis?
Get in touch with our expert staff and book an appointment today. Our experts can get your feet feeling like they should!
Summerside Location
Westbrook Location
Heel Pain Cause #2: Heel Fat Pad Syndrome/Fat Pad Atrophy (FPA)
What is it?
Heel Fat Pad Syndrome is the second most common cause of heel pain behind plantar fasciitis. Our heels absorb a lot of weight and provide our bodies with a lot of cushioning. Between our heel bone and our skin lies a fat pad. This fat pad acts as a shock absorber to cushion the blow from repetitive heel strikes when walking, running, jumping, and standing.
What causes heel fat pad syndrome? What are the symptoms of heel fat pad syndrome?
Similar to plantar fasciitis, damage to the fat pad can occur with overuse. Recent weight gain, an increase in load on the heel and lack of range of motion at the ankle can all contribute to fat pad syndrome.
Unlike plantar fasciitis, heel fat pad syndrome can also be worse at night and with rest due to the inflammatory nature of the condition (Interestingly, plantar fasciitis, despite the “itis” that implies inflammation, is usually absent of inflammatory markers). Heel fat pad syndrome may also cause pain more in the middle of the heel, whereas plantar fasciitis can be more commonly felt in the front inside portion of your heel bone. Fat pad syndrome may also present with numbness and tingling into the heel. Fat pad syndrome also tends to be more common in both feet as opposed to one single foot.
What can I do to fix my heel pain from fat pad syndrome?
Activity modification, wearing footwear with a supportive heel at all times, specific exercises and a form of “low dye” taping of the heel can also be used to help manage your heel pain from fat pad syndrome.
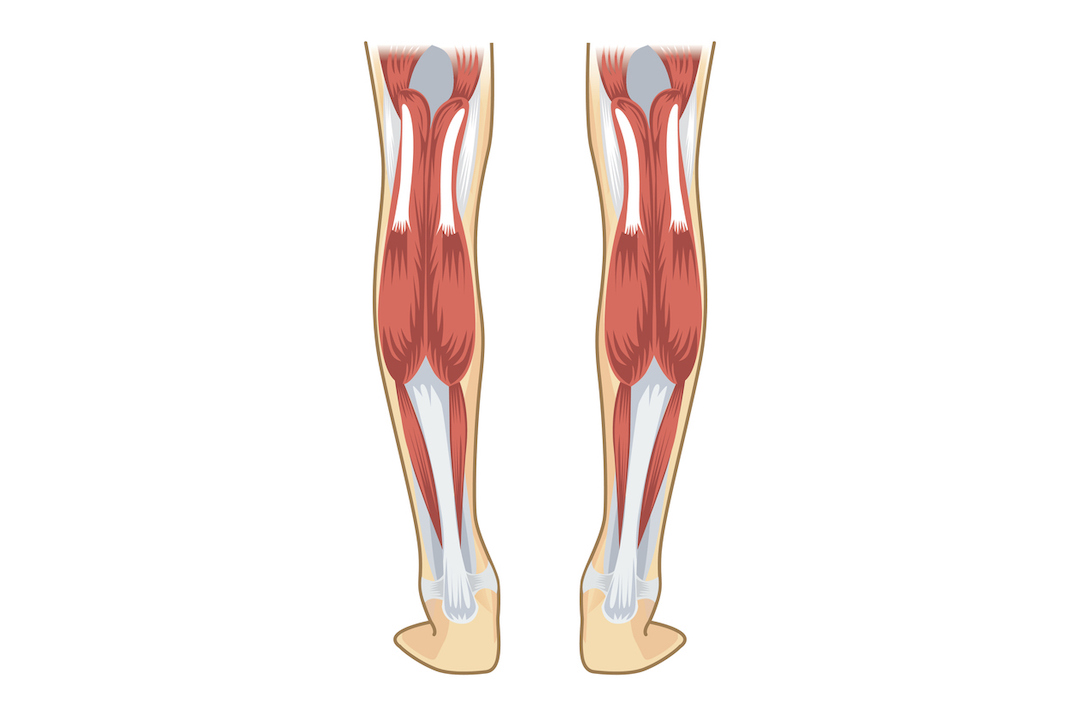
Heel Pain Cause #3: Short or “Tight” Calf Muscles.
What is it?
When muscles in the calf become shortened or tight, either due to injury or adaptation to your activities of daily living, a tipping point can be reached. When this occurs, they calf muscles can refer pain down through the achilles tendon into your heel. This results in heel pain. In this case, the heel is the “victim” but the calf muscles are the culprit.
What are the symptoms of tight calf muscles causing heel pain?
Similar to plantar fasciitis, the pain is localized to the bottom of the heel/foot. The pain can also be worse first thing in the morning, or when active for long periods. However, unlike plantar fasciitis, if you tiptoe walk first thing in the morning when your heel pain is at its worst, your pain would likely lessen or go away. If this happens, your care plan may be better suited at targeting your calf muscles first as opposed to your heel. In this case, the therapists at REP Physio will provide you with exercises and stretches that focus on your calf. Activity modification, soft tissue massage, and intramuscular dry needling are great options for care for heel pain due to tight calf muscles.
What can I do to fix my heel pain from “tight” calf muscles?
Check out our video below for some common stretches that form part of the plantar fascia/heel pain protocol at REP Physio.
Cause #4: Referral from your lower back (really).
Yup, in some cases, the pain in your heel may be referred from your lower back. This type of heel pain may often be accompanied by numbness, tingling and/or altered sensation (paresthesia) into the lower leg and foot. Clinically we refer to this as a radiculopathy. Radiculopathy is a term to describe a range of symptoms due to a nerve being pinched or compressed as it exits the spine. In the case of your heel pain, it is often compression to the S1 nerve root in your back that causes heel pain. Said differently, your back is the “culprit”, and your heel is the “victim”.
What are the symptoms of heel pain coming from my lower back? How is it caused?
You may experience a burning sensation or a deep throb, and/or numbness and tingling into your lower leg, heel and foot. Unlike plantar fasciitis and or tight calves, you can also feel pain in the bottom of your heel when you are at rest. In fact, in some cases, sitting down may make your heel feel worse if your referred pain is discogenic in nature. Heel pain coming from your lower back tends to affect only one side. The therapists at REP Physio will be able to do a thorough orthopedic and neurologic examination and determine if your heel pain is coming from your back and provide you with the tools you need to make your heel (and back!) feel better.

Heel Pain Cause #5: Heel Bone Fractures (Traumatic or Stress Fracture)
A substantial fall from a height onto your heels can certainly give rise to the possibility of an acute fracture of the calcaneus (heel) bone. If you have recently fallen from a height and are experiencing heel pain, come see one of the therapists at REP Physio if you haven’t already been to the hospital of seen your physician. We’ll assess you and determine if X-rays are required to rule in/out a heel fracture. If a fracture is found, our therapists are experienced at rehabilitating you once it is safe to do so.
What are the symptoms of a fracture causing heel pain? How can I fix it?
Stress fractures to the heel bone are an uncommon source of heel pain. Often a stress fracture may have similar symptoms to plantar fasciitis. In this case a careful examination and discussion about your heel pain is required. If a stress fracture is suspected, the physiotherapists at REP Physio will discuss medical imaging options with you. Stress fractures are typically managed by immobilizing the heel in a boot and/or using crutches to off-load the heel for 6-12 weeks.
Can I blame my shoes for my heel pain?
Oftentimes, shoes are blamed for heel pain. New shoes, old shoes, low heels, high heels, no heels etc.. Generally speaking, heel pain is due to the stress placed on your tissues, not the footwear you are in. In fact, there is limited evidence that shoe cushioning (type) can reduce the incidence of running injury/heel pain. Your therapist at REP Physio will happily discuss with you your current shoe situation and can also discuss if you would be a candidate for different shoes and/or orthotics (rarely).
Heel Pain Cheat Sheet
Heel Pain Type | Activity | Rest | Pain Location | Pain Quality | Onset |
|---|---|---|---|---|---|
Plantar Fasciitis | Worse, esp. in the a.m. Walking: better | Better | Front of heel, may extend to toes Unilateral more common | Sharp, esp. in the morning | Gradual |
Fat Pad Syndrome | Worse Walking: worse | Worse Night pain | Middle of heel Bilateral more common | Bruise-like tingling, aching, cold | Gradual |
Tight Calves | Worse | Better | Entire heel Uni/bilateral | General soreness | Gradual |
Pinched Nerve | Better or worse | Worse if you are sitting (discogenic) | Entire heel Unilateral more common | Dull/throb Numb/burning Tingling | Gradual or following back injury |
Fracture | Worse | Better | Varies Unilateral or bilateral | Sharp | Trauma (acute) Gradual (stress) |
References:
B. Dubois. “New Trends in the Prevention of Running Injuries” The Running Clinic 2010.
M. Thomas et al. “Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use.” BMC Musculoskeletal Disorders Vol 20:337 (2019)
B. Buchanan, D. Kushner. “Plantar Fasciitis” Statpearls 2021 June 5. Accessed 11 August 2021 https://www.ncbi.nlm.nih.gov/books/NBK431073/
J. Kirkpatrick et al. “The plantar calcaneal spur: a review of anatomy, histology, etiology and key associations.” Journal of Anatomy 230:6 743-751. 2017.
Heel Fat Pad Syndrome. Physiopedia.com/Heel_Fat_Pad_Syndrome#cite_note-:0-4 Accessed 11 August 2021


