Headaches are a common complaint we see at REP Physio. Studies show that 46% of us can expect to have a headache(s) within a year, while 64% of us will experience headache(s) during our lifetime (1). There are many distinct types of headaches and causes. In fact, the International Classification of Headache Disorders manual, which details known headache types is over 200 pages!(2) What follows is a brief guide explaining the characteristics of some of the more common types of headaches we see at REP Physio. As always, if you have concerns about your health, seek out a qualified health professional.
When is a Headache a Medical Emergency?
Sometimes a headache can be a sign of a more severe problem including a stroke, meningitis, extremely high blood pressure, as well as other diseases such as cancer. In this regard, it is generally best to seek immediate medical attention if:(3)
It is the first severe headache you have ever had, and it significantly interferes with your life
It is accompanied by slurred speech, facial paralysis, and/or an inability to lift your arms above your head
It occurs with a fever, stiff neck and nausea
Your headache comes on quickly and is explosive and violent
Your headache occurs with head injury
You experience a severe new headache and are immunocompromised (HIV) and/or have a history of cancer
Major Headache Types: Primary or Secondary Headaches
Headaches can be classified as either primary or secondary.
A primary headache is due to the headache itself. There are 3 types of primary headaches:
- Migraine
- Tension type headaches (TTH) (also known as muscle tension headaches)
- Cluster headaches
A secondary headache is one that develops due to another cause. For example, a sinus headache due to sinusitis, or a hangover headache due to consuming too much alcohol.
Primary Headaches (Headache due to the headache itself)
1. Migraines
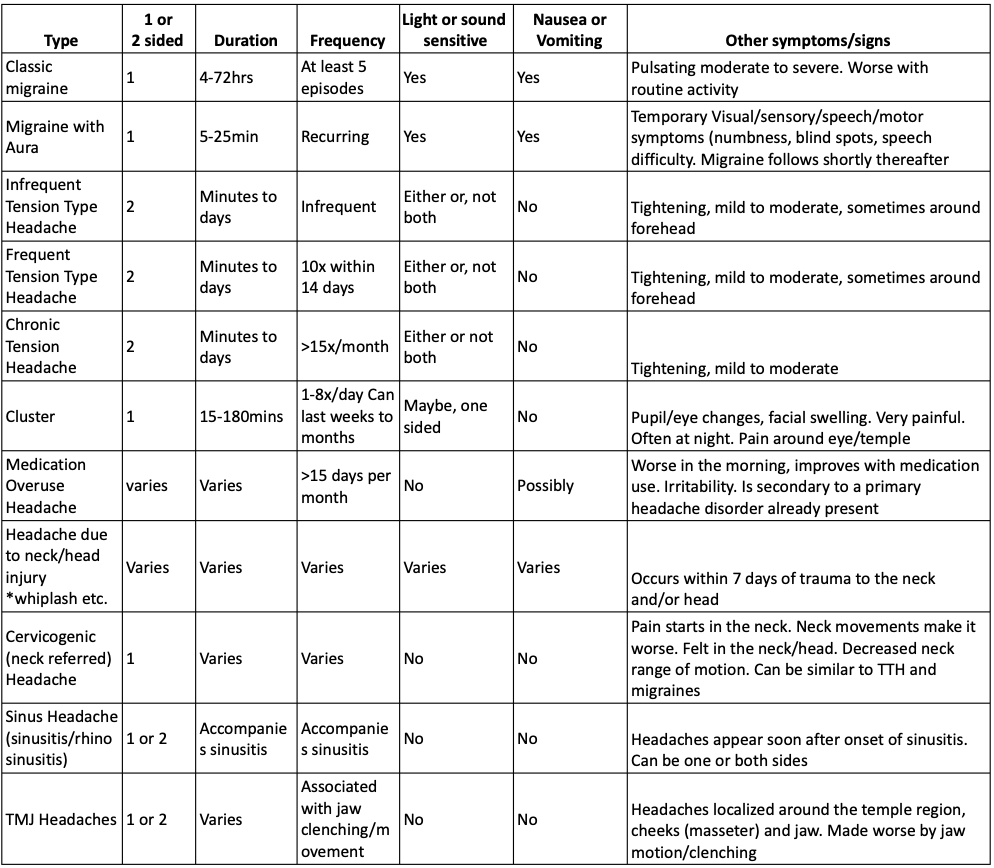
Migraines without aura (Classic Migraine):
A recurrent headache disorder (at least five episodes) manifesting in attacks lasting 4-72 hours. Classic migraines are typically unilateral (one-sided), are pulsating in nature, and are of moderate or severe intensity. It can be aggravated by routine physical activity. During a classic migraine, at least one of the following is also present: Nausea or vomiting is typically present, and or sensitivity to light and sound.
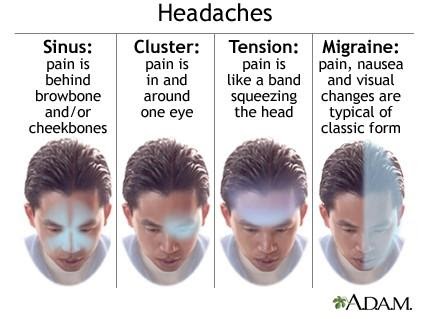
Image courtesy of: https://medlineplus.gov/ency/article/000797.htm (16)
Migraines with aura:
Recurrent attacks, lasting minutes, of unilateral, fully reversible, visual, sensory or other central nervous system symptoms that develop gradually and are usually followed by headache and associated migraine symptoms.(4) The “aura” refers to temporary disturbances to visual and motor systems (difficulty with speech, visual changes, numbness, weakness). Typically, these disturbances associated with this type of headache last between 5 to 30 minutes and are followed by a headache about an hour later.
Unfortunately, the causes of migraines are not fully understood. Genetics and environmental factors may play a role.(5) Some factors that can influence migraines include Stress, hormonal changes, alcohol/caffeine consumption, physical exertion, weather changes, foods and food additives among many others.
Type 1: Infrequent Tension Type Headaches: (ITTH)
ITTHs are identified by infrequent episodes of headache (<1x/month), typically on both sides of the head that are pressing or tightening in quality and of mild to moderate intensity. ITTHs last minutes to days. Headache symptoms do not worsen with routine physical activity and are not associated with nausea. Light or sound sensitivity (not both) may be present.(6) The area around the skull may or may not be tender.
Type 2: Frequent Tension Type Headaches (FTTH)
FTTHs are identical in presentation to infrequent tension type headaches but must include 10 episodes of headache occurring on 1-14 days/month on average for greater than 3 months.(7)
Type 3: Chronic Tension Type Headaches (CTTH)
CTTHs share all the features of Frequent Tension Type Headaches, except the headaches occur on greater than 15 days per month on average for greater than 3 months.(8)
Unfortunately, the causes of TTHs are not totally clear. Previously it was associated with muscle contractions and/or tension in the neck, jaw and face, but that does not seem to be the sole (or primary) cause. Current research is pointing towards a higher “sensitivity” of the nervous system (sensitization) and pain receptors that can magnify pain symptoms as a cause of tension type headaches.(9) This may also explain the tenderness you feel around the skull or “pericranial” area. Stress appears to be one of the most common triggers of tension type headaches.
3. Cluster Headaches
Cluster headaches include attacks of severe, one-sided pain around the eye and/or in the temple (side of head) region. Cluster headaches typically last 15 minutes to 180 minutes and can occur from 1-8 times per day. Cluster headaches can last from weeks to months, followed by periods of remission.(10)
They often wake people at night. People with cluster headaches may also demonstrate same side enlarged eye blood vessels, enlarged or shrunken pupils, increased tearing, a runny nose and/or congestion. Same sided facial swelling and or sweating may also be present. People with cluster headaches may also experience agitation and restlessness.(11) The cause of cluster headaches is unknown, but research is pointing towards changes in the hypothalamus (the body’s biological clock) as being a potential cause.(12)

Secondary Headaches (Headache due to another cause, i.e., a hangover)
1. Medication Overuse Headache/ Rebound Headache:
Medication overuse headaches (MOH), also known as rebound headaches typically occur in people with a pre-existing primary headache disorder. MOHs occur greater than 15 days per month and develop as a consequence of regular overuse of headache medication and pain relievers for greater than 3 months. Medication overuse headaches usually resolve once the medication overuse is stopped. More than half of individuals with headaches greater than 15 days per month are attributable to medication overuse.(13)
2. Headaches due to Trauma to the Neck/Head (Concussion, Whiplash etc.)
This type of headache is identifiable by an onset close in time (within 7 days) to trauma to the neck or head. A whiplash injury or concussion are common causes of this type of headache. The injury does not have to be severe for this type of headache to occur. These headaches can be short term, or chronic (>3 months duration). Research suggests that the cause of these headaches may be due to inflammation around the axons (nerves) around the brain and or altered brain metabolism post-trauma.(14)
3. Cervicogenic Headaches
Cervicogenic headaches are one-sided and usually start with neck pain. The pain is typically made worse by positions and/or movements of the neck. It can also be accompanied by reduced range of motion of the neck. Putting pressure on one side of the neck may also make the headache symptoms worse. The symptoms can refer to the head and face. With cervicogenic headaches, the pain should resolve within 3 months following treatment of the affected structures in the neck (joints and or soft tissue in the upper neck).(15) This can be done with soft tissue massage, specific exercise and/or manual therapy provided by your physiotherapist at REP Physio.
4. Sinus Headaches
Sinus headaches can accompany rhinosinusitis (sinusitis). Rhinosinusitis refers to inflammation of the sinus and nasal cavities. Headaches of this type typically occur soon after the onset of rhinosinusitis. They tend to worsen when the rhinosinusitis worsens and can also be made worse when pressure is applied around the nasal sinuses. Sinus headaches are felt around and above the nose on one or both sides.
5. Temporomandibular Joint (TMJ) Headaches
Headaches of this type are due to joint and soft-tissue dysfunction about the jaw. It can be made worse by jaw motion and/or clenching of the jaw and grinding of the teeth. Symptoms of TMJ headaches typically occur around the temple region, jaw and cheek.
Techniques to Relieve Headaches
Keep a headache diary to manage and help identify potential triggers.
Minimize alcohol and caffeine consumption.
Practice good sleep hygiene. Go to bed and wake up on a regular schedule. Avoid screen time prior to going to bed
Work on relaxation techniques to reduce stress. Mediation, yoga or other activities you find relaxing are good options. If managing stress is difficulty for you, contact REP’s psychologist Dr. Thamarai Moorthy at 780 395 9170.
Exercise on a regular basis. Our physiotherapists and personal trainer can get you set up with a program that meets your unique needs.
Eat a healthy diet. If you have questions about your diet, contact REP’s dietitian Sabina Valentine at sparkes@ualberta.ca
See a physiotherapist for the management of your headache symptoms. At REP Physio we are trained in identifying and treating common types of headaches. If your headache is not one that physiotherapy can help, we will work with you to identify the most appropriate course of action.
References:
- G. Manzoni, L Stovner, “Epidemiology of Headaches," Handbook of Clinical Neurology 2010;97:3-22
- Headache Classification Committee of the International Headache Society (IHS). “The International Classification of Headache Disorders, 3rd Edition.” Cephalalgia, vol.38(1) 1-211, 2018, pp1-211. Doi: DOI: 10.1177/0333102417738202
- No Author “Headaches Danger Signs.” Medline Plus https://medlineplus.gov/ency/patientinstructions/000424.htm Accessed 3 November 2021
- IHS. “The International Classification”, p.18
- No Author. “Migraine,” Migraine, Mayo Clinic 2 July 2021 Accessed 28 October 2021. https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201
- IHS. “The International Classification”, p 35
- Ibid. p.36
- Ibid. p.37
- No Author. “Tension Headache” Tension Headache, Mayo Clinic 29 September 2021 Accessed 28 October 2021. https://www.mayoclinic.org/diseases-conditions/tension-headache/symptoms-causes/syc-20353977
- No Author. “Cluster Headache” Cluster Headache, Mayo Clinic 24 July 2021 Accessed 28 October 2021. https://www.mayoclinic.org/diseases-conditions/cluster-headache/symptoms-causes/syc-20352080
- Ibid.
- Ibid.
- IHS “The National Classification”, p. 122
- IHS “The National Classification”, p. 149
- Yasir Al Khalili et al. “Cervicogenic Headache” Cervicogenic Headache, National Library of Medicine January 2021. Accessed 4 November 2021. https://pubmed.ncbi.nlm.nih.gov/29939639/
- Image courtesy of: https://medlineplus.gov/ency/article/000797.htm Accessed 3 November 2021
